Results from Canada's first Accountable Care Unit

Top Results
Overview
In a study conducted at Pasqua Hospital in Regina, Saskatchewan, the implementation of Canada’s first Accountable Care Unit (ACU) led to significant improvements in length of stay, and patient and staff satisfaction.
Objectives
To determine the feasibility of implementing an ACU in a Canadian hospital and to assess its impact on various outcomes including length of stay, readmissions, mortality, patient and staff satisfaction.
Methods
The study was conducted on Ward 4A, a 35-bed medicine/family medicine unit at Pasqua Hospital. The ACU model included:
Unit-based physician teams
Structured Interdisciplinary Bedside Rounds (SIBR)
Unit-based performance reports
Unit-level nurse-physician leadership dyads
The study compared 6-month data from the ACU with a control unit, as well as baseline data pre- and post-ACU implementation. Data sources included Health Information Management Services, the Patient Advocate Office, and a Team STEPPS 2.0 survey.
Results
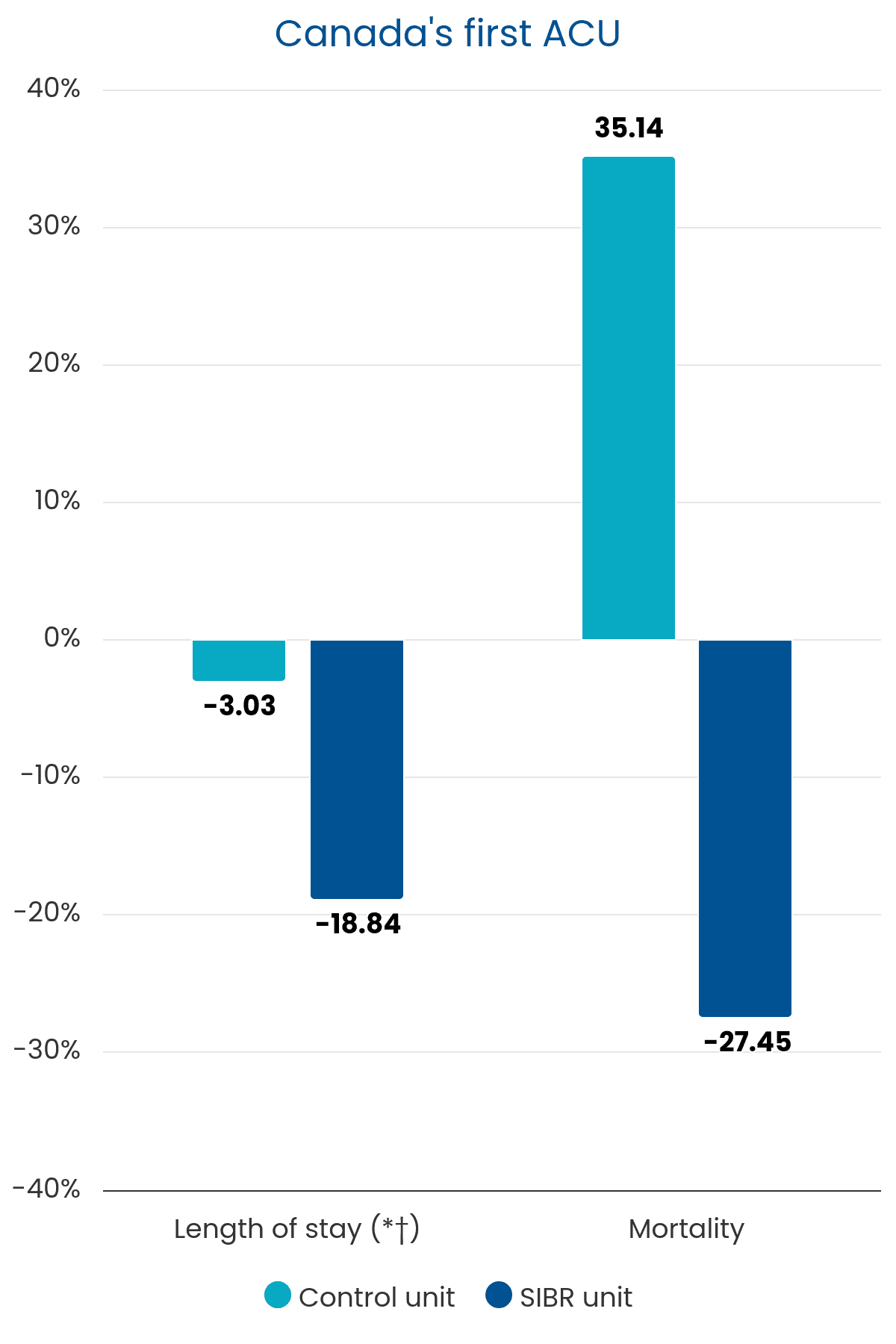
Length of Stay (LOS):
Decreased by 18.84% (from 8.65 to 7.02 days, P<0.05) on the ACU ward.
Control ward saw a 3% reduction (from 8.57 to 8.31 days, P=0.64).
30-Day Readmissions:
Decreased from 15.7% to 13.3% on the ACU ward.
Control ward decreased from 13% to 11.7%.
Mortality:
Decreased from 5.1% to 3.7% on the ACU ward.
Control ward saw an increase from 3.7% to 5.0%.
Patient Satisfaction:
• Significant improvements in decision making, safety, pain management, care and treatment, and patient-centered care (P<0.05).
Client Advocacy Complaints:
Reduced from 16 to 7 on the ACU ward (P<0.05).
Control ward saw a reduction from 16 to 14.
Staff Satisfaction:
Improved in staff-supervisor relations (+22%) and perceptions of care provided (+17%) (P<0.05).
Nursing Overtime Costs:
Decreased from $18,100 to $11,700 per month on the ACU ward.
Control ward decreased from $17,500 to $15,300.
Process Outcomes:
The interdisciplinary team spent an average of 51 minutes on SIBR for 14 patients per day.
A targeted date of discharge was verbalized 97% of the time during SIBR.
Clinical Performance Outcomes:
Improvements in documentation of VTE prophylaxis rationale, urinary catheter rationale, pneumococcal vaccination, malnutrition screening, nutritional monitoring, and patient weighing (P<0.05).
Conclusion
The implementation of the ACU at Pasqua Hospital demonstrated the feasibility and positive impact of the ACU model in a Canadian hospital setting. Significant improvements were observed in length of stay, patient satisfaction, and staff satisfaction, with trends toward reduced mortality and readmissions. Based on these results, the ACU model is being expanded to other units within Pasqua Hospital and additional hospitals in Saskatchewan.