Interdisciplinary Plan of Care (IPOC): a valuable tool for aligning care teams in a complex world

Background
An interdisciplinary plan of care (IPOC) is a coordinated approach to patient care that involves healthcare professionals from different disciplines working together to develop and implement a comprehensive integrated plan tailored to a patient's specific needs. This approach is particularly important in modern healthcare where patient numbers and their complexity continues to rise and the resources available to treat is ever decreasing: a single healthcare provider's ability to treat is insufficient to efficiently address all aspects of the patient's health needs and discharge.
Key Aspects of an Interdisciplinary Plan of Care
Collaborative Team:
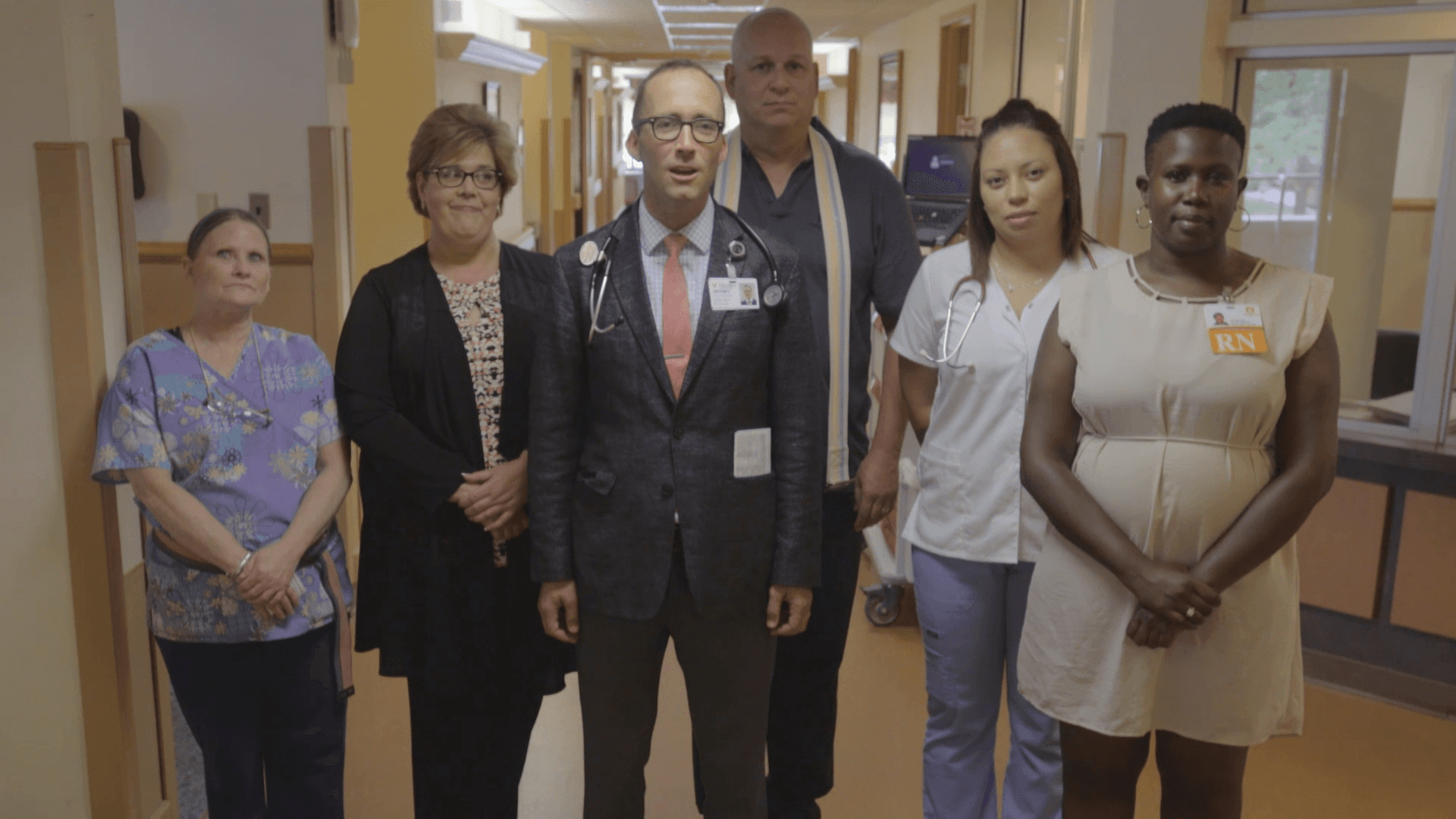
The care team typically includes a variety of healthcare professionals including doctors, nurses, social workers, physical therapists, occupational therapists, dietitians, and other specialists.
Each team member contributes their expertise to address different aspects of the patient's care, such as medical treatment, barriers to discharge, rehabilitation, psychosocial support, and nutrition.
Comprehensive Assessment:
The team conducts a thorough assessment of the patient's needs. This might involve evaluating medical history, current symptoms, functional status, mental health, and family dynamics.
The patient and their family are also involved in the assessment to ensure that the care plan aligns with the patient's preferences and goals.
Goal Setting:
Based on the assessment, the team should collaboratively set SMART goals specific for the patient’s care: specific, measurable, achievable, relevant, and time-bound. These goals address the various domains of the patient’s well-being and are tailored to their unique circumstances.
Goals can range from symptom management and improving mobility to enhancing quality of life or preparing for discharge.
Care Plan Development:
The interdisciplinary team develops a detailed plan of care that outlines interventions, responsibilities, and timelines. Each team member has a specific role in executing the plan, as well as the patient and/or their family.
The plan is dynamic and can be adjusted as the patient's condition evolves or as new information becomes available.
Communication and Coordination:
Effective communication is critical for the success of an IPOC. Regular meetings or interdisciplinary rounds are held where team members discuss the patient’s progress, challenges, and any necessary adjustments to the care plan.
Clear documentation and information sharing ensure that all team members are updated and that care is consistent.
Patient-Centered Approach:
The patient is at the center of the IPOC. Their preferences, values, and cultural beliefs are respected and integrated into the plan of care.
Patient and family education is an essential component, helping them understand the care plan and participate actively in the care process.
Evaluation and Adjustment:
The team regularly evaluates the effectiveness of the care plan in achieving the set goals. If the patient’s needs change or if certain interventions are not as effective as expected, the plan is adjusted accordingly.
Continuous evaluation helps in delivering high-quality care that adapts to the patient's evolving condition.
Benefits of an Interdisciplinary Plan of Care:
Holistic Care: Addresses all aspects of a patient's health and well-being.
Improved Outcomes: The coordinated approach can lead to better health outcomes, reduced complications, and enhanced patient satisfaction.
Efficiency: Reduces redundancy and ensures that all aspects of care are covered without overlap.
Enhanced Communication: Facilitates better communication among healthcare providers, patients, and families, leading to more cohesive care delivery.
Common Settings for IPOC:
Hospitals: Especially in units like ICU, oncology, or rehabilitation where patients have complex needs.
Long-term care facilities: For residents with chronic conditions requiring ongoing multidisciplinary management.
Home care: Where care is coordinated across various professionals visiting the patient at home.
Palliative care: Where managing symptoms, providing psychosocial support, and improving quality of life are primary goals.
How Structured Interdisciplinary Bedside Rounds (SIBR rounds) support the development of patient IPOCs
SIBR rounds are an innovative approach to enhancing the coordination of care in hospital settings. These rounds support the development and implementation of Interdisciplinary Plans of Care (IPOCs) by fostering real-time, collaborative decision-making at the patient’s bedside through:
1. Real-Time, Collaborative Decision-Making
SIBR rounds involve a multidisciplinary team of physicians and nurses, and will often include pharmacists, case managers/social workers, or therapists, depending on the unit's resources. This team meets at the patient's bedside, at a set frequency and time, to discuss the patient’s current status and care plan.
This real-time, face-to-face collaboration ensures that all team members contribute their expertise simultaneously, allowing for immediate adjustments to the care plan based on the latest information.
As the patient and their family are typically included in these discussions, the patient’s preferences and concerns are directly integrated into the IPOC, making it truly patient-centered.
2. Structured Communication
SIBR rounds are highly structured, following a standardized format that ensures that all relevant aspects of the patient’s care are discussed. This might include discussing the patient’s current condition, overnight events, progress toward goals, upcoming procedures or tests, and discharge planning.
The structured nature of SIBR rounds helps prevent critical information from being overlooked and ensures that all team members are on the same page.
This structure supports the development of a comprehensive and well-coordinated IPOC by systematically addressing all necessary components of the patient’s care.
3. Enhanced Coordination and Accountability
By bringing the entire care team together regularly (usually daily) at the bedside, SIBR rounds enhance coordination across disciplines. Team members can immediately address any discrepancies or issues in the care plan, reducing the likelihood of miscommunication or redundant efforts.
Each team member's role in the IPOC is clarified during SIBR, and responsibilities are assigned and confirmed, increasing accountability.
This high level of coordination helps ensure that the IPOC is not only well-designed but also effectively executed.
4. Continuous and Dynamic Updating of the Care Plan
One of the challenges in traditional care planning is the lag between patient assessment, care team communication, and updating the care plan. SIBR rounds address this by allowing the care plan to be continuously reviewed and updated in real time as a team and with the patient or family.
If new information or changes in the patient’s condition arise, the IPOC can be immediately modified during the SIBR rounds, ensuring that the care plan remains relevant and effective.
This dynamic updating process is crucial in managing complex patients whose conditions may change rapidly.
5. Patient and Family Engagement
SIBR rounds actively involve the patient and their family in the care discussion, giving them a voice in the planning process. This ensures that the IPOC aligns with the patient’s goals and preferences, increasing their satisfaction and adherence to the care plan.
Engaging the patient and family also helps clarify any questions they may have, ensuring they understand the care plan and their role in it.
Engaging the patient and family with respect to the discharge plan enables the discharge destination to be determined early in the hospitalization, improving the discharge efficiency.
6. Reduction of Silos in Care Delivery
Traditional care often occurs in silos, with each discipline working independently. SIBR rounds break down these silos by fostering interdisciplinary communication and collaboration at the bedside.
This integration helps in creating a more holistic IPOC that considers all aspects of the patient’s health, from medical management to psychosocial support.
7. Improved Quality and Safety of Care
The SIBR model has been associated with improvements in clinical outcomes, including reductions in length of stay, readmissions, and adverse events. By ensuring that all team members are aligned and aware of the care plan, the likelihood of errors or omissions is reduced.
A safer, more effective care environment supports the execution of the IPOC, ensuring that the patient receives the highest quality care.
Keep Exploring Our Work



